Dreaming After TBI
DREAMING IS A COMPLEX AND MYSTERIOUS ASPECT OF human consciousness, with dreams offering a window into our unconscious mind. While the exact functions of dreams remain elusive, they are considered essential for emotional processing, memory consolidation and even problem-solving. However, when it comes to traumatic brain injury (TBI), the effects on dreaming are not well understood. TBI, which occurs due to an external force to the head, can cause a range of cognitive, emotional and physical impairments. It can also have a profound impact on the dreaming process, which is intricately tied to the brain’s ability to function. This article explores how TBI affects dreaming, the changes in dream patterns and the potential reasons behind these alterations.
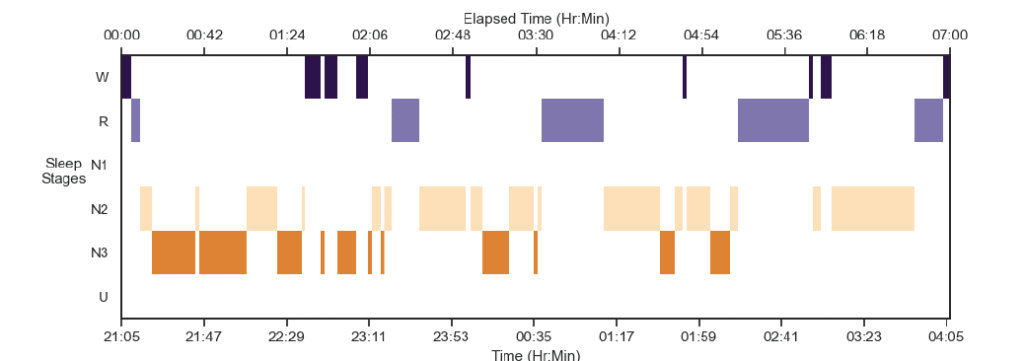
Sleep stages graph (hypnogram) above shows the different stages of sleep of participants during their session.
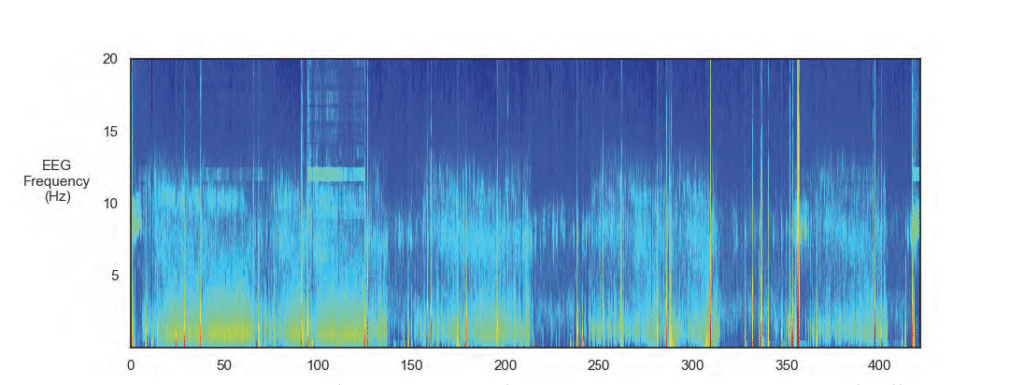
The EEG spectogram image above shows the intensity of brainwave activity over time. High-intensity regions are indicated by tones of red, yellow and green, and low-intensity regions are indicated by tones of blue.
UNDERSTANDING DREAMING AND THE BRAIN
Dreams are primarily associated with rapid eye movement (REM) sleep, a stage of sleep that is crucial for restorative processes in the brain. During REM sleep, brain activity is high, and the brain undergoes various functions, including the processing and consolidation of memories. It is during REM sleep that vivid and often surreal dreams occur. Non-REM sleep stages, especially deep sleep, also play a role in memory consolidation, physical restoration and the maintenance of cognitive functions.
The brain structures that play an essential role in dreaming include the prefrontal cortex, the limbic system (which controls emotions) and the hippocampus (which is involved in memory formation). These regions work together to create the vivid scenarios that we experience while dreaming. Traumatic brain injury can disrupt these brain structures, resulting in changes to the dreaming process, affecting both the content and quality of dreams.
THE IMPACT OF TBI ON DREAMING
The effect of TBI on dreaming varies depending on the severity of the injury, the regions of the brain affected and whether the individual is recovering from the injury. However, several common trends have emerged in research that help to explain the link between TBI and changes in dreaming.
Disruption in REM Sleep
One of the primary effects of TBI on dreaming is a disruption of the sleep cycle, especially REM sleep. Many individuals with TBI report experiencing difficulty entering or maintaining REM sleep, which in turn affects the intensity and frequency of dreams. Some individuals with TBI may experience less REM sleep overall, which reduces the opportunity for dreaming. On the other hand, some individuals report fragmented or disrupted REM sleep, leading to sleep disturbances that may cause nightmares or vivid dreams.
The disturbance in REM sleep following TBI is often linked to the brain’s inability to regulate sleep cycles effectively. Damage to brain regions such as the hypothalamus, which controls the circadian rhythm, and the brainstem, which regulates REM sleep, can result in sleep fragmentation and other disturbances that affect dreaming.
Changes in Dream Content
The content of dreams can be profoundly altered after a traumatic brain injury. Dreams may become more bizarre, fragmented or distressing. Some individuals with TBI report an increase in violent or frightening dreams, including nightmares, possibly due to heightened emotional responses to stress or trauma experienced during the injury. The emotional part of the brain, particularly the amygdala, may be affected by TBI, which could make emotions such as fear, anxiety and anger more dominant in dreams.
Moreover, people with TBI may experience more frequent dreams that revolve around the injury itself or the events surrounding it. These types of dreams may be related to post-traumatic stress, a common condition following a TBI. Dreams may replay the traumatic incident or present variations of the injury experience, leading to increased distress and anxiety. Such dreams are often reflective of the brain’s attempt to process and integrate traumatic memories.
Sleep Apnea and Other Sleep Disorders
Sleep disorders, including sleep apnea, are common in individuals with TBI. Sleep apnea is a condition in which a person’s breathing repeatedly stops and starts during sleep. This leads to reduced oxygen levels in the blood, further disrupting the sleep cycle and negatively affecting REM sleep. The lack of quality REM sleep can significantly impact dreaming, causing a reduction in dream intensity or altering the nature of dreams.
TBI can contribute to the development of sleep apnea by affecting the brainstem, which plays a role in regulating breathing. In addition to sleep apnea, other sleep disorders such as insomnia and restless leg syndrome may also develop after TBI, further affecting sleep quality and, by extension, the dreaming process.
NEUROCHEMICAL CHANGES AND THEIR EFFECT ON DREAMS
The brain’s neurotransmitter systems play a crucial role in regulating sleep and dreaming. TBI can result in alterations in the levels of neurotransmitters such as serotonin, dopamine and acetylcholine, which are all involved in the regulation of sleep and dream activity. Damage to these systems may lead to abnormal sleep cycles, less REM sleep and changes in the emotional tone of dreams.
Serotonin, for example, is critical for maintaining healthy sleep patterns and mood regulation. TBI-related disruptions in serotonin levels may contribute to sleep disturbances, nightmares and emotional instability in dreams. Similarly, changes in dopamine levels can affect motivation, reward systems and mood regulation, leading to more vivid or unusual dreams. Alterations in acetylcholine, a neurotransmitter essential for REM sleep, can directly impact the quality and frequency of dreaming.

NEUROPLASTICITY AND DREAMING POST-TBI
Neuroplasticity, the brain’s ability to reorganize itself and form new neural connections, plays a role in recovery after a traumatic brain injury. As the brain heals and compensates for areas of damage, it may restore some functions, including the ability to engage in normal sleep cycles and experience regular dreams. However, the extent of this recovery depends on the severity of the injury, the areas of the brain affected and the individual’s age and overall health.
In some cases, as neuroplasticity allows the brain to compensate for damage, individuals with TBI may experience a return of more vivid or coherent dreams. Conversely, some individuals may experience persistent disruptions in dreaming as the brain continues to adapt to the injury. The process of neuroplasticity is unique to each individual, and its impact on dreaming remains an area of ongoing research.
POTENTIAL TREATMENTS FOR DREAMING DISTURBANCES FOLLOWING TBI
While there is no definitive treatment to restore normal dreaming after a traumatic brain injury, several strategies may help manage the associated sleep disturbances and improve sleep quality, which, in turn, can support healthier dreaming.
Cognitive Behavioral Therapy for Insomnia (CBT-I): This type of therapy is often used to treat sleep disturbances in individuals with TBI. CBT-I helps individuals identify and address thoughts and behaviors that interfere with sleep, leading to improvements in overall sleep quality, which may also have a positive effect on dreaming.
Pharmacological Interventions: Medications such as antidepressants, antianxiety drugs or sleep aids may
be prescribed to individuals with TBI who suffer from nightmares or other sleep disturbances. These medications may help to regulate sleep patterns and reduce the frequency of nightmares.
Relaxation Techniques: Techniques such as meditation, deep breathing and progressive muscle relaxation may help individuals with TBI reduce stress and anxiety before sleep, leading to improved sleep quality and potentially less disturbing dreams.
Sleep Hygiene Education: Establishing a consistent sleep routine and creating a calm and comfortable sleep environment can improve sleep quality, leading to better recovery and less disruption to dreaming. Sleep hygiene strategies may include maintaining a consistent sleep-wake cycle, avoiding caffeine and alcohol before bedtime and minimizing screen time in the hours leading up to sleep.
Nightmare Management: Individuals who suffer from frequent nightmares related to TBI may benefit from therapies that focus on trauma resolution, such as EMDR (eye movement desensitization and reprocessing) or trauma-focused cognitive-behavioral therapy. These approaches aim to reduce the emotional impact of traumatic memories, potentially decreasing the frequency and intensity of nightmares.
IN CONCLUSION
The effects of traumatic brain injury on dreaming are varied and complex, reflecting the intricate nature of the brain’s sleep and memory systems. TBI can lead to disruptions in REM sleep, changes in dream content, increased nightmares and memory difficulties related to dream recall. These disturbances are influenced by various factors, including neurochemical changes, emotional responses to trauma and disruptions in brain regions responsible for sleep regulation.
Although many individuals with TBI experience significant changes to their dreams, there are effective strategies for managing these disturbances, including cognitive behavioral therapies, pharmacological interventions and lifestyle changes. By addressing the underlying sleep issues, it is possible to improve sleep quality, reduce nightmares and enhance the overall healing process following a traumatic brain injury. As research into the relationship between TBI and dreaming continues, a better understanding of these processes may lead to more targeted treatments and interventions.
Contribute to the TBI Times