Diagnosing TBI can be complicated. Currently, doctors use a variety of methods to determine if a patient has a TBI. A medical exam is the first step to diagnose a potential brain injury which includes a neurological exam. This exam evaluates thinking motor function, sensory function, coordination, eye movement, and reflexes. Although it is well acknowledged within the medical community that they can not detect TBIs, CT and MRI scans are typically the next step because they can rule out a more serious brain injury. Although these protocols aid health care providers who are trained in the intricacies of diagnosing TBIs, none on their own can provide a definitive diagnosis. However, there is promising research showing that more advanced imaging may take center stage in the diagnosis of both TBI and mTBI (mild traumatic brain injury).
This next-level imaging falls into two categories: Nuclear Medicine in the form of single-photon emission computerized tomography (SPECT) and positron emission tomography (PET) scans and Diffusion Tensor Imaging (DTI) scans.
SPECT AND PET SCANS
SPECT is a nuclear imaging scan that integrates computed tomography (CT) and a radioactive tracer. The tracer is what allows doctors to see how blood flows to brain tissue. Before the SPECT scan, a tracer is injected into your bloodstream. The tracer is radiolabeled, meaning it emits gamma rays that can be detected by the CT scanner. The computer collects the information emitted by the gamma rays and displays it on the CT cross-sections. These cross-sections can be added back together to form a 3D image of your brain. The radioactive tracers will pass through your body and be detected by the scanner.
PET scans also use radiotracers however for additional purposes other than monitoring blood flow. PET scans also visualize and measure and physiological processes such as regional chemical composition and absorption. In both SPECT and PET scans, different tracers are used depending on the purpose of the scan. In the case of TBI screening, Fluorodeoxyglucose (FDG) is the most widely used radiotracer.
A SPECT scan differs from a PET scan in that with SPECT the tracer stays in your bloodstream rather than being absorbed by surrounding tissues, thereby limiting the images to areas where blood flows. SPECT scans are cheaper and more readily available than higher resolution PET scans, though both scans can detect minute molecular biological changes in the brain, which is not possible for MRI or CT scans.
According to Dr. Daniel Amen, a brain health expert, “Brain SPECT imaging identifies areas of the brain hurt by TBI. CT and MRI scans show if there is any damage to the anatomy or structure of your brain, but these scans cannot tell how your brain is functioning. In fact, after a TBI, CT or MRI scans will often appear normal when there is actually functional damage to the brain that can be detected with SPECT.”
DTI SCAN
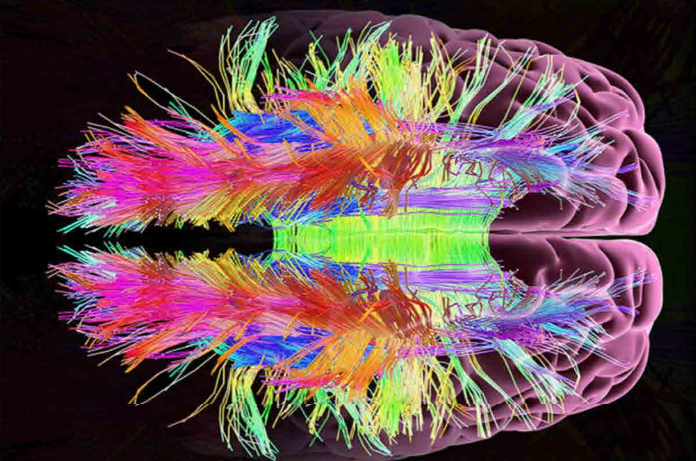
DTI scans are a relatively new magnetic resonance imaging (MRI) technique that is used to evaluate microstructural changes in the brain by measuring water molecules in tissue. Its imaging capabilities are based on the ability to determine the orientation and diffusion characteristics of white matter. Recent advances in the resolution of DTI have made it possible to visualize potential changes in various neural tracts associated with brain injury. DTI is used in conjunction with conventional MRI techniques to provide 2-dimensional and 3-dimensional visualization of changes to white matter in the brain. DTI scans can provide image contrast that was previously unattainable using conventional MRI techniques.
According to Lauren J. O’Donnell, PhD of the Golby Neurosurgical Brain Mapping Laboratory, DTI is a sensitive probe of cellular structure that works by measuring the diffusion of water molecules. Unlike the diffusion in a glass of pure water, which would be the same in all directions (isotropic), the diffusion measured in tissue varies with direction (is anisotropic). The measured macroscopic diffusion anisotropy is due to microscopic tissue heterogeneity. In the white matter of the brain, diffusion anisotropy is primarily caused by cellular membranes, with some contribution from myelination and the packing of the axons. Anisotropic diffusion can indicate the underlying tissue orientation.
WHAT ADVANCED IMAGING TECHNIQUES MEAN FOR TBI PATIENTS
Being able to thrive with TBI means getting the proper diagnosis, which is the first step in getting the appropriate treatment. SPECT, PET, and DTI scans are making this possible for more patients. The amount of detail and diagnostic information made available by these scans can help doctors create very customized treatment plans for patients with TBI.
With more research being done every year to develop advanced imaging modalities, the future is definitely brighter for patients suffering from TBI.