Mild or moderate COVID-19 lasts about two weeks for most people. But in some, the long-term effects of COVID-19 can cause lingering health problems and wreak havoc for months. Tae Chung, M.D., a specialist in neurology and physical medicine and rehabilitation; Megan Hosey, Ph.D., an expert in rehabilitation psychology; Arun Venkatesan, M.D., Ph.D., a specialist in neurology; Amanda Morrow, M.D., an expert in pediatric rehabilitation medicine; and Ann M. Parker, M.D., Ph.D., who specializes in lung disease and critical care, discuss long-term COVID-19, what symptoms are most common and what those affected by them can expect Mild or moderate COVID-19 lasts about two weeks for most people. But others experience lingering health problems even after the fever and cough go away and they are no longer testing positive for the illness. Parker notes that the World Health Organization has developed a definition for post-COVID-19 condition (the WHO’s term for long COVID) as coronavirus symptoms that persist or return three months after a person becomes ill from infection with SARS CoV-2, the coronavirus that causes COVID-19. Those symptoms can include fatigue, shortness of breath and cognitive problems. The symptoms can come and go, but have an impact on the person’s everyday functioning, and cannot be explained by another health problem. WHAT CAUSES POST-COVID SYNDROME? While it’s clear that people with certain risk factors (including high blood pressure, smoking, diabetes, obesity and other conditions) are more likely to have a serious bout of COVID-19, there isn’t a clear link between these risk factors and long-term problems. In fact, long COVID can happen in people who have mild symptoms, although patients with more severe initial illness seem to be more likely to have long-term impairments. More studies will shed light on why these stubborn health problems persist in some people. SARS-CoV-2 can attack the body in a range of ways, causing damage to the lungs, heart, nervous system, kidneys, liver and other organs. Mental health problems can arise from grief and loss, unresolved pain or fatigue, or from post-traumatic stress disorder (PTSD) after treatment in the intensive care unit (ICU).
Doctors are seeing a spectrum of symptoms after acute COVID-19, some of which would be expected after other critical illnesses. Some are minor, but other people may need continuing care and even readmission to the hospital. Similar, lingering problems can affect patients with other serious illnesses. But it is notable that post-COVID-19 syndrome is not just afflicting people who were very sick with the coronavirus: Some patients who were never severely ill with COVID-19 are experiencing long-term symptoms. DO COVID VACCINES PREVENT LONG COVID? Getting vaccinated for COVID-19 lowers the risks of COVID infection. While breakthrough infections are possible, being fully vaccinated and boosted is effective in reducing the risk of hospitalization and death due to COVID. Research is ongoing about how long COVID affects people who had breakthrough COVID, but it is likely that being vaccinated reduces the risk. POST-COVID SYNDROME CONDITIONS The senses of smell and taste are related, and because the coronavirus can affect cells in the nose, having COVID-19 can result in lost or distorted senses of smell (anosmia) or taste. Before and after people become ill with COVID-19, they might lose their sense of smell or taste entirely, or find that familiar things smell or taste bad, strange or different. For about a quarter of people with COVID-19 who have one or both of these symptoms, the problem resolves in a couple of weeks. But for most, these symptoms persist. Though not life-threatening, prolonged distortion of these senses can be devastating and can lead to lack of appetite, anxiety and depression. Some studies suggest that there’s a 60% to 80% chance that these people will see improvement in their sense of smell within a year. Neurologist Arun Venkatesan, M.D., Ph.D., says, “Some individuals develop medium to long-term symptoms following COVID infection, including brain fog, fatigue, headaches and dizziness. The cause of these symptoms is unclear but is an active area of investigation
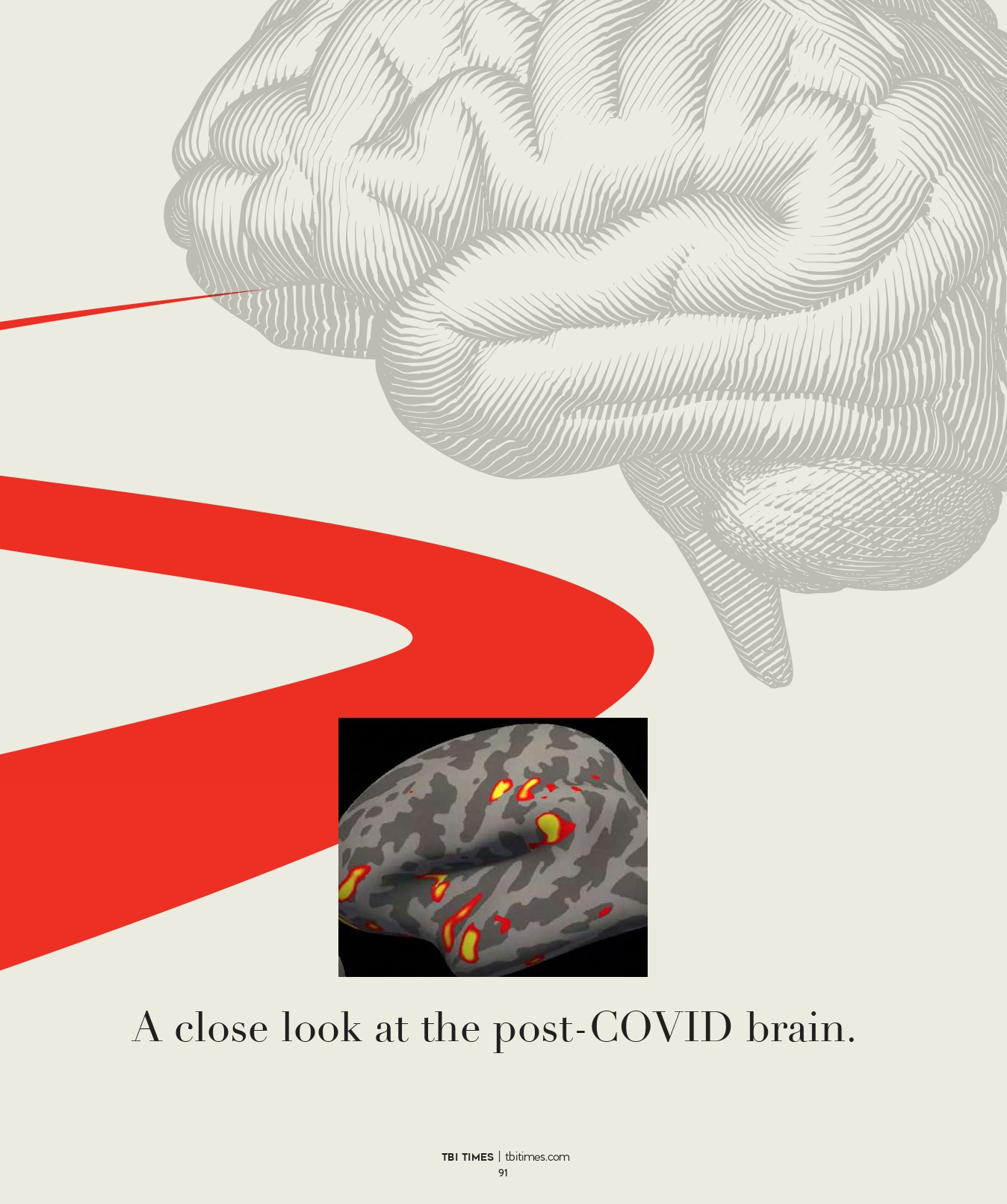
THE STUDY, INVOLVING PEOPLE AGED 51 TO 81, FOUND SHRINKAGE
AND TISSUE DAMAGE PRIMARILY IN BRAIN AREAS RELATED TO
SENSE OF SMELL; SOME OF THOSE AREAS ARE ALSO INVOLVED
IN OTHER BRAIN FUNCTIONS
Can COVID-19 increase a person’s risk for anxiety, depression and cognitive issues? A study of COVID-19’s impact on mental and emotional well-being conducted by Johns Hopkins experts in psychiatry, cognition (thinking, reasoning and remembering) and mental health found that these problems were common among a diverse sample of COVID-19 survivors. Cognitive impairment after acute coronavirus infection can have a severe impact on a person’s life. Long-haul COVID patients may experience changes in the way they think, concentrate, speak and remember, and these symptoms can affect their ability to work or even maintain activities of daily living. After recovering from the coronavirus, some people are left with lingering anxiety, depression and other post-COVID mental health issues. Physical changes such as pain and weakness can be complicated by long periods of isolation, stress from job loss and financial difficulties, and grief from the deaths of loved ones and the loss of good health. The relationship between COVID-19 and diabetes, especially type 2 diabetes, is complex. Type 2 diabetes is a risk factor for serious cases of COVID-19, and some survivors of the illness seem to be developing type 2 diabetes signs after they recover from COVID-19. It’s not yet known whether children who have had COVID-19 are more or less likely than adults to experience continuing symptoms. But long-term COVID-19 in children is a possibility, showing up as fatigue, headaches, difficulty with school work, mood concerns, shortness of breath and other long-hauler symptoms

